The Problems with Pepcid and other antacids, Part 1
By Laurie Goldstein, September 2015
One of the most common health-related medicinal recommendations I see for cats experiencing gastrointestinal issues such as nausea, inappetence, and “overnight bile pukes” is Pepcid a/c (famotidine). And why not? It is perceived to be very safe, many vets recommend it, and antacids generally are easy to obtain all around the world. Call the vet first! They’ll probably say it’s OK to give it a try, and it often does (seem to) help. This is because acid suppression can address the symptoms and our uncomfortable kitties feel better and begin to eat or stop throwing up. Sometimes just stopping the cycle of nausea and inappetence for a couple of days is enough to turn the tide when your cat is feeling poorly. Short-term, occasional or intermittent use of antacids is not the issue.
Long-term use is.
Note: The manufacturers of the over-the-counter antacids do not recommend use longer than two weeks at a time without consulting a physician, and Prilosec (omeprazole) is not intended for more than two weeks of use every four months. Our vets and our doctors often fail to mention this.
So what are the problems?
Because we are led to believe they are completely safe, many cats are given antacids frequently, regularly, and have been on antacids long term to soothe upset tummies. And we may unintentionally and unknowingly be contributing to our kitties’ illness.
How are antacids making some cats sick?
The gastrointestinal tract is technically outside of the body. It is a giant hole, a passageway that snakes from mouth to anus filled with barriers to prevent unintentional movement from “outside” to “inside.” It is segmented with a system of valves to prevent “backflow” and isolate contents of one section from another until an appropriate time. Its purpose is not only to process nutrients we ingest, but to prevent infection from bacteria, viruses, parasites, and all the many toxins to which we are exposed. By its very nature, the GI system must account for the bulk of our immune system defense. Estimates of that percentage range from 70% to 80%: either way, the health of the GI tract and maintaining those barriers in proper condition is absolutely critical to overall health. The low pH of stomach acid and the low average pH of the stomach contents is one of the very first lines of that defense system.
Problem 1: Taking medications that constantly neutralize or block stomach acid production interfere with the body’s normal immune defenses.
The higher-than-normal pH created by the antacids is associated with
– C difficile infection
– bacterial overgrowth
– small intestinal bacterial overgrowth (SIBO), and
– bile acid deconjugation, a common (and often undiagnosed) cause of chronic diarrhea and fat malabsorption.
Problem 2: Antacids interfere with nutrient absorption.
Have you ever prepared bone broth? Add a dash of apple cider vinegar (which is 5% – 7% acetic acid), and your broth softens the bones faster. Same principle here: stomach acid is needed to prepare vitamins and minerals for absorption, and has a critical role in B12 metabolism. With acid suppression, the pH of the stomach increases and the absorption of nutrients becomes impaired due to what is basically improper preparation. Decades of research show that low stomach acid (whether natural or induced by medication) reduces absorption of:
– Iron
– Calcium
– Zinc
– Folate (Vitamin B9, Folic Acid)
– B12 (Vitamin B12, Cobalamin)
– Vitamin D
Problem 3: Motility and muscle tone.
The higher pH of the stomach artificially created by antacids results in delayed gastric emptying times (gastroparesis). This can cause
– Further increased stomach pH
– upper abdominal pain
– loss of appetite
– changes in blood sugar levels
– feeling full after eating only a little bit.
It has also been demonstrated that the cascade of chemical impacts from the higher-than-normal gastric pH can cause an abnormally relaxed ileocecal valve, leading to translocation of bacteria from the large intestine into the small intestine, which enables SIBO (see above).
Problem 4: Chronic Kidney Disease (CKD)/Chronic Renal Failure (CRF) and aging kitty antacid toxicity
Antacids can become toxic if not used at reduced levels and/or reduced intervals in cats with kidney disease or in kidney failure due to slower renal clearance and longer drug half-life. The same is true in older cats due to altered physiology (water/fat/muscle mass changes due to age) that results in higher blood plasma concentrations. In fact, the manufacturers of antacids specifically recommend lower doses for humans with impaired renal function – yet as in people, these cautions are often overlooked in caring for our cats.
Other Antacids
There are two primary classes of acid suppressing medications:
1) H2 Blockers (H2 antagonists): Pepcid a/c (famotidine); Zantac (ranitidine); Tagamet (cimetidine)
2) Proton Pump Inhibitors (PPIs): Prilosec (omeprazole), Nexium (esomeprazole), Protonix (pantoprazole), and Prevacid (lansoprazole).
The H2 blockers like Pepcid are not the worst offenders when it comes to acid suppression, and all of the H2 blockers are available over-the-counter (at pharmacies without a prescription). Although the risks are generally the same for both classes of acid suppressants (and the risk of toxicity the same for kidney disease or renal failure), the probability of experiencing these unhealthy and unwanted side-effects are greater with the proton pump inhibitors like Prilosec (omeprazole) (see references).
PPIs inhibit acid secretion more effectively than H2 blockers which is why they are carry a higher risk of any or all of these associated problems. Omeprazole (Prilosec) is the only one of the PPIs sold at pharmacies without a prescription, and dosages for cats can (unfortunately) easily be found online.
These studies are in humans – why does this matter to my cat?
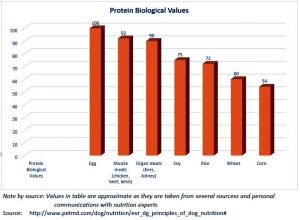
The basic chemical and neurological signaling mechanisms in the gastrointestinal tract are similar in cats and humans. This is why antacids designed for humans work to suppress stomach acid in cats and why we use them in the first place. Although there are no studies of the impact of acid suppressants in cats, the naturally low gastric pH is potentially more important for our obligate carnivores – especially if fed a fresh, species-appropriate food:
– Gastric pH acts as an ecological filter, preventing harmful bacterial infection and protecting the healthy balance of bacteria needed to support nutrient metabolism and overall health.
– Gastric pH impacts motility, and normal intestinal motility is a major defense mechanism against attachment of pathogenic bacteria in the small intestine.
– Low gastric pH is essential for cleaving B12 from the amino acids in meat;
The low gastric pH is needed to properly metabolize minerals (let alone derive those minerals from bone).
This is why we need to approach Pepcid a/c (famotidine), Zantac (ranitidine) and PPIs like Prilosec (omeprazole) with caution. There is a place for these drugs in the short term care of cats in gastric distress, no doubt. But ultimately the solution is to understand and cure or mitigate the underlying problem, rather than continue to mask it with a remedy that might be making your cat sicker in the long term.
I know – those of you who have cats with kidney disease are saying, “But there is no cure.” In Part 2, we share research that indicates most cats with kidney disease (unlike dogs and humans with CKD or CRF) suffer a nausea that is related to uremic toxins, not excess gastric acid, and is best treated centrally, not with antacids.
If my cat hasn’t been diagnosed with GERD, what are my treatment options? In Parts 2 and 3 we will discuss alternatives to antacid medications for managing kitty’s nausea and vomiting.
References
Ahn JS et al 2013. Acid suppressive drugs and gastric cancer: a meta-analysis of observational studies, World J Gastroenterol Apr 28:19(16):2560-8 (2013). http://www.ncbi.nlm.nih.gov/pubmed/23674860
Beasley et al 2015. The Evolution of Stomach Acidity and Its Relevance to the Human Microbiome, PLoS ONE 10(7): e0134116. doi:10.1371/journal.pone.0134116 (2015). http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0134116
Carter D et al 2013. Prevalence and predictive factors for gastrointestinal pathology in young men evaluated for iron deficiency anemia, May: 58(5):1299-305 (2013). http://www.ncbi.nlm.nih.gov/pubmed/23192647
Cheungpastiporn W et al 2015. Proton pump inhibitors linked to hypomagnesemia: a system review and meta-analysis of observational studies, Aug: 37(7):1237-41 (2015). http://www.ncbi.nlm.nih.gov/pubmed/26108134
Dukowicz AC et al 2007. Small Intestinal Bacterial Overgrowth: A comprehensive review, Gastroenterol Hepatol (NY), Feb: 3(2):112-122 (2007). http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3099351/
Gallieni M & Cancarini G 2015. Drugs in the Elderly with Chronic Kidney Disease, Nephrol Dial Transplant, 30(3):342-344 (2015). http://www.medscape.com/viewarticle/842049
Islam RS and DiBaise JK 2012. Bile Acids: Nutrition Issues in Gastroenterology, Series #110, Practical Gastroenterology (October 2012). http://www.medicine.virginia.edu/clinical/departments/medicine/divisions/digestive-health/nutrition-support-team/nutrition-articles/Parrish_Oct_12.pdf
Jameson R et al 2013. Proton Pump Inhibitor and Histamine 2 Receptor Antagonist Use and Vitamin B12 Deficiency, JAMA 310(22):2435-2442 (2013). http://jama.jamanetwork.com/article.aspx?articleid=1788456
Lo WK and Chan WW 2013. Proton pump inhibitor use and the risk of small intestinal bacterial overgrowth: a meta-analysis, Clin Gastroenterol Hepatol May: 11(5):483-90 (2013). https://www.ncbi.nlm.nih.gov/pubmed/23270866
Lombardo L 2010. Increased incidence of small intestinal bacterial overgrowth during proton pump inhibitor therapy, Clin Gastroenterol Hepatol Jun: 8(6): 504-8 (2010). http://www.ncbi.nlm.nih.gov/pubmed/20060064
Manlucu et al 2005. Dose-reducing H2 receptor antagonists in the presence of low glomerular filtration rate: a systematic review of the evidence, Nephrol Dial Transplant, Nov:20(11):2376-2384 (2005). http://ndt.oxfordjournals.org/content/20/11/2376.full
Mora JR and von Andrian UH 2009. Role of retinoic acid in the imprinting of gut-homing IgA-secreting cells, Seminars in Immunology 21:28-35 (2009). http://vonandrian.hms.harvard.edu/Publications/2009/Mora_2009.pdf
Marcuard SP et al 1994. Omeprazole Therapy Causes Malabsorption of Cyanocobalamin (Vitamin B12), Annals of Internal Medicine, Vol 120, No. 3 (Feb 1994). http://annals.org/article.aspx?articleid=707082
Parkman HP et al 1998. Effect of gastric acid suppressants on human gastric motility, Gut 42:243-250 (1998). http://m.gut.bmj.com/content/42/2/243.full
PennState-Hershey, Milton S. Hershey Medical Center. Ulcer Medications – histamine H2 antagonists. http://pennstatehershey.adam.com/content.aspx?productId=107&pid=33&gid=000219
Roulet L et al 2012. Adverse effects of proton pump inhibitors: should we worry about long term exposure? Rev Med Interne Aug: 33(8):439-45 (2012). http://www.ncbi.nlm.nih.gov/pubmed/22284952
Russell RM et al 1988. Effect of antacid and H2 receptor antagonists on the intestinal absorption of folic acid, J Lab Clin Med Oct: 112(4):458-63 (1988). http://www.ncbi.nlm.nih.gov/pubmed/2902178
Shindo K & Fukumura M 1995. Effect of H2-receptor antagonists on bile acid metabolism, J Investig Med, Apr: 43(2)170-7 (1995). http://www.ncbi.nlm.nih.gov/pubmed/7735920
Thorens J et al 1996. Bacterial overgrowth during treatment with omeprazole compared with cimetidine: a prospective randomized double blind study, Gut 39:54-59 (1996). http://gut.bmj.com/content/39/1/54.full.pdf
Tleyjeh IM et al 2013. The Association between Histamine 2 Receptor Antagonist Use and Clostridium difficile Infection: A Systematic Review and Meta-analysis. PLoS ONE, 2013; 8 (3): e56498. http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0056498
Vadokas B et al 1997. Effects of gastrin-releasing peptide (GRP) on the mechanical activity of the human ileocaecal region in vitro, Neurogastroenterology & Motility Dec: 9(4):265-270 (1997). http://onlinelibrary.wiley.com/doi/10.1046/j.1365-2982.1997.d01-59.x/abstract
Vighi et al 2008. Allergy and the gastrointestinal system, Clin Exp Immunol 153 (Suppl 1): 3-6 (2008 Sep). http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2515351/
Wilhelm SM et al 2013. Perils and pitfalls of long-term effects of proton pump inhibitors, Expert Rev Clin Pharmacol, Jul: 6(4):443-51 (2013). http://www.ncbi.nlm.nih.gov/pubmed/23927671
The Problem with Pepcid, Part 2: How to identify & manage nausea in your cat
By Laurie Goldstein, September 2015
In Part 1, we discussed how long term use of antacids may raise stomach pH, which can cause
– bacterial infection, bacterial overgrowth, small intestinal bacterial overgrowth (SIBO),
– bile acid deconjugation (a common and often diagnosed cause of fat malabsorption and chronic diarrhea, distinguished by yellow or green watery stool);
– nutrient deficiencies, notably B12, iron, calcium, zinc, folate, and vitamin D; and
– reduced gastric emptying times. Delayed gastric emptying can result in pain, loss of appetite, feeling full after eating only a little bit, and changes in blood sugar levels.
It is important to note that these are risks, not givens, and that the probability of problems is higher with proton pump inhibitors (like Prilosec (omeprazole)) than with the H2 blockers (like pepcid a/c (famotidine) and Zantac (ranitidine)). Antacids can safely be used short term to stop a cycle of nausea and inappetence; sometimes a few days is all that is needed. If it isn’t, then it is best to identify and address the underlying cause. Obviously, treating the cause is always better than treating the symptoms when possible, and apart from treating stomach ulcers and/or rare hyperacidity, all other uses of antacids simply suppress symptoms. Of course antacids can be used for longer periods, and the H2 blockers have a lower probability of the side-effects occurring compared to the proton pump inhibitors, but such use should only be done with vet awareness and supervision despite the availability of these drugs without prescription. That said, here in Part 2, we focus on how to identify and address the source of the nausea rather than just suppress the symptoms.
Identifying Nausea and GI Distress
It is quite common to think one’s cat is being finicky when the problem is actually nausea. Part of the problem is that there is no one symptom that is specific to nausea, and cats, of course, are well known for hiding any illness or injury if they can.
Any one (or combination) of these symptoms can indicate your cat is feeling nauseous:
Loss of appetite
Acting hungry but walking away from food
Just licking at or sniffing food
Head hanging over water dish but not drinking
Vomiting water
Vomiting frothy foam (bile) (it can be white, yellowish, or tinted red)
Lip licking or lip smacking (which can be a sign of nausea OR dehydration)
Drooling
Eating grass or plants
Pica, often licking or nibbling plastic, eating plastic plants
Sitting in a “meatloaf” position (see pictures, below)
Howling/Yowling (often indicates pain if such vocalizations are not normal in your cat)
Immediately regurgitating after eating
Of course, most things on this list can have a different cause at their source. This is one of the great difficulties when trying to diagnose and treat cats. Many problems present the same symptoms, and each set of symptoms may indicate a variety of potential problems. No matter the cause, if kitty is displaying any of these symptoms in combination with behavior that indicates she isn’t feeling well, a vet trip is in order. Don’t let paranoia take over, but with cats, a touch of paranoia is better than putting off a vet trip until a problem reaches obviously serious status.
Behavior that indicates any of the above symptoms are related to illness:
Changes in litter box habits (eliminating out of the litter box)
Changes in bowel movements or urination frequency
Changes in social interaction (hiding or not interacting with you or other pets as they normally do; aggression on petting or brushing can indicate pain)
Changes in activity (lethargy – cats don’t usually slow down much as they age; more activity – this can be caused by hyperthyroidism)
Changes in sleeping habits
Changes in grooming habits (greasy or matted fur; dandruff; reduced grooming)
Changes in vocalization
Bad breath (this can be related to a dental problem or a GI problem).
Too many times, people, even vets, may think a problem is just “old age,” but that is rarely the case in cats. Remember that cats are usually not fond of change, so when they change in appearance or behavior, there is likely to be a specific cause. We often don’t observe our fur companions closely until they get sick, but it’s helpful to take note of body language now so you’ll know when something isn’t right. It is the same with blood tests. A test done while a cat is healthy supplies a baseline for later. It’s one thing to know what the lab norms are, but just as in people, “normal” varies at times from cat-to-cat. Know your cat’s normal so when kitty is “off” the change in blood values can be identified. A physical exam, blood work, perhaps an x-ray, and/or an abdominal ultrasound will be a part of the diagnostic process.
Note: Vomit that looks like coffee grounds means there is active bleeding in the stomach, often from ulcers. This is an emergency, and you should get kitty to your vet or an emergency vet as soon as possible. Red tinged vomit indicates ruptured capillaries in the esophagus and is usually from the irritation to the throat from vomiting. This is of concern if it happens frequently, but again, a vet check is always best.
Meatloafing: comparing comfortable positions with those indicating nausea
The every-day meatloafs
There are four basic “meatloaf” positions. The first two pictured here are normal, every-day positions; the final two are indications your cat feels sick and/or is in pain.

Happy, relaxed, not nauseous:

Not necessarily relaxed, this pose says “this is my spot.” But it doesn’t indicate nausea.

Looks uncomfortable, possibly in pain, head down

Clearly uncomfortable, sitting forward on haunches, in pain, sometimes with head down, eyes squinted.
Treating Nausea and Vomiting: Food
Apart from using medicine (prescription or over-the-counter) there are three basic components of treating GI problems in your cat: food, supplements, and water. We also address hairballs, a common cause of nausea and vomiting in cats.
Food
Issues that can cause GI problems:
1. What is fed
2. How it is fed
3. When it is fed
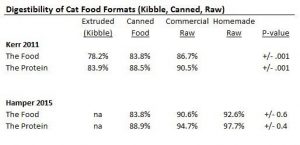
What is Fed
Cats are obligate carnivores. Their natural diet consist of small prey animals. Some argue they naturally consume carbohydrates because of the stomach and intestinal contents of the prey. An examination of the diet of feral domestic cats (that have access to very little human food or garbage) found the stomach contents of prey provide very little in the way of carbs: just 2% of the diet on an energy basis. This author notes that the contents of the stomach and intestines are, for the most part, predigested. Thus feeding our cats a species-appropriate (low carb, grain-free, meat-and-organ based) diet can be the difference between a sick kitty and a healthy kitty. Some food companies and vets maintain that cats can metabolize carbs, which they can. But there is a big difference between “can” and “should.” Also, there remains a question of at what point carbs become a problem. For those that want to stick with commercial diets, a food that contains 40% carbohydrates (usually measured on a dry matter basis, a downloadable carb calculator in Excel is available, here) is simply not going to be a good long term choice. When making food choices, bear in mind that vets that embrace our kitties as the obligate carnivores they are, but are not anti-carbs in their diet, usually suggest no more than 20% of the diet be carbs. There is no research to indicate one way or another whether that level of non-meat based ingredients will take a toll on your kitty’s organs over time or not. One thing is clear: the physiology of a cat indicates they are not intended to derive much energy or nutrition from grain-based foods or intake of carbohydrates. Feed low carbs.
If cats were in charge of the pet food industry, cat food instructions would likely read, “remove mouse, rabbit or small bird from freezer: thaw and serve.” Anything else is 1) for our convenience, 2) due to our access to feeding resources, or 3) due to the cost of feeding. When our cats get sick, we need to learn how to best balance our time and resources with their needs. So please know that:
⦁ Grains can cause nausea and vomiting.
⦁ Non-grain carbohydrates such as peas can cause nausea and vomiting. This is tricky, because many Limited Ingredient Diets contain peas to raise the protein level and lower the cost. Anecdotally, we’re finding more and more IBD cats reacting to the peas in the food.
⦁ Otherwise high carb foods can cause nausea and vomiting. Many “grain-free” foods simply replace grains with non-grain starches. The problem? Carbohydrate ingestion does not trigger the same gastric secretion as meat-based proteins. A high carb diet can raise stomach pH, leading to improperly digested protein and/or delayed gastric emptying, contributing to nausea and/or vomiting.
⦁ A carb “red flag:” Meat is high in methionine, an amino acid used by many companies as a urine acidifier. If the synthetic version, “DL-methionine” is supplemented, especially if you find it towards the top of the supplement list in commercial food ingredients, alarm bells should go off; this is an indication the food does not contain protein primarily from meat or that the food is otherwise high in carbohydrates. Those carbs make the entire GI system, not just the stomach, too alkaline, and this can lead to various issues, among them urinary tract health problems and the formation of crystals. Natural methionine is found in meat, one of the reasons a meat-based diet naturally targets the proper pH in cats.
⦁ The many thickeners in most commercial canned foods can cause nausea, vomiting, and GI irritation. Thickeners and gelling agents include carrageenan, xanthan gum, guar gum, locust bean gum, cassia gum, agar agar, tapioca, potato starch, and wheat gluten. This list is not complete, but these are common additives for thickening and gelling. Any or all of them can cause stomach upset and nausea.
⦁ Food/ingredient sensitivities can cause nausea and vomiting.
⦁ Food allergies can cause nausea and vomiting. Grains are a common culprit. A frequently-fed protein can be the cause.
⦁ Kibble is often a culprit. Whether it is problem ingredients, the highly processed nature of kibble, or its impact on stomach pH and motility (due to being free-fed no matter the quality of ingredients – see Hairballs, below), simply removing kibble from the diet provides relief in many cats.
How Kitty is Fed
⦁ Raise the dishes. Cats normally eat sitting or standing so their throat is at the same height or lower than the stomach. If kitty does have problems with acid reflux, raising the food and water dishes to head-height (while sitting up or standing) can resolve this problem. In Part 1 we discussed how acid reflux is not caused by excess acid; it is a problem with muscle tone in the lower esophageal sphincter, the valve that is meant to prevent stomach acid from rising into the throat. By keeping the head elevated and letting gravity work, the raised dishes keep the stomach acid in the tummy. Once there is food in the stomach, the acid is put to work.
⦁ Slow kitty down. When a cat eats too fast and regurgitates as a result, this is almost always when kitty is being fed kibble. Rather than put a rock or ball in the dish to slow down kitty, please just stop feeding kibble. If kitty manages to wolf down food so fast they regurgitate canned, homecooked, or raw food, then portion out smaller amounts and extend meal time to numerous smaller meals over 10 or 15 minutes vs one plop of food in a dish left out for 10 to 15 minutes. (And bless you for having adopted a formerly abused cat or kitty rescued from a hoarding situation, as this is behavior displayed most often by cats in those situations. Feral cats that almost starved usually slow down pretty quickly on their own once they realize food is provided regularly. Please don’t underrate the importance of emotions and psychology in cats. Please take the time to treat the whole kitty, and that’s more than just the body).
When Kitty is Fed
⦁ Feed smaller, more frequent meals. Two meals a day is not ideal for cats. Their systems are geared toward eating more frequent smaller meals (as in the wild they hunt small prey). Add a meal as late as possible before you go to bed. Reducing the length of time between the last meal of the day and the first meal of the next day often stops overnight bile pukes.
⦁ Feed a freeze dried meat treat to kitty when you get up, and/or prior to bed, and/or in the middle of the night, and/or prior to meals. The anticipation of food gets the gastric juices flowing. Giving kitty a protein-based meat treat that puts those gastric juices to work can stop the morning (or overnight) bile pukes, and can stop the regurgitation of the morning meal. In some cases, a middle of the night treat will resolve pre-breakfast vomiting better than any medicine. For those making a trip to the bathroom in the middle of the night, taking the time to give kitty a treat can improve your cat’s morning – and yours as well. If bile pukes happen during the day, or meal regurgitation is a frequent occurrence, feed kitty a few small bites of freeze-dried meat treats as needed, when you get home from work, or about 10 to 15 minutes before each meal to see if that resolves the problem. Pure Bites, Whole Life, and Grandma Lucy’s are popular brands of single-ingredient meat treats made in the USA.
⦁ Stop free-feeding and move to timed meals. (Better yet, stop the kibble). In cats, indigestible solids (such as hair) are the last items to leave the stomach. They are forced out of the stomach only by the strong peristaltic waves created by hunger pangs. If kitty is never hungry, motility is impaired and waste material does not move through kitty’s system properly. Obviously this can cause nausea, and a belly full of hair or improperly digested food can cause a loss of appetite as kitty feels full. (For transition tips and how to help kitty understand the concept of meal time, please see Transitioning to Timed Meals OR New Food)
⦁ For more on the timing of meals for kitty, please see How often should you feed your cat?
Hairballs
Hairballs are by far the most common cause of nausea, inappetence and vomiting in cats. And yet hairballs are NOT normal. I know it’s news to many. But a healthy cat does not normally have anything other than an occasional hairball, and tossing a hairball more than twice a month in long-haired cats and more than once every two months in short-haired cats can be indicative of GI disease. A study published in 2014 found that 99 of 100 cats examined for chronic vomiting – including tossing hairballs – had GI disease. Of those 99 cats, 50 had some form of cancer, and 49 had some form of inflammatory bowel disease. Many may still joke about hairballs, but hairballs are NOT a joke.
A primary symptom of hairballs is regurgitating undigested food hours after eating. Prior to this point, kitty feeling full and seeming “picky” about eating can be a subtle sign of hairballs:
1. Cats with hairballs often seem “picky” but otherwise fine: they don’t necessarily display any signs of nausea other than wanting to eat but not eating;
2. Kitty regurgitating the meal undigested hours after eating is often hungry immediately, and displays no other behavioral signs of illness.
To address hairballs in our cats, it is best to:
⦁ Stop free feeding and feed timed meals (addressed above)
⦁ Stop feeding kibble (feed canned, cooked, or raw food – food with moisture)
⦁ Feed species-appropriate food (low carbohydrate, no grain foods, addressed above)
⦁ Forget the petromalt or petroleum-based hairball products. It is best to address hairballs by treating the underlying problem: GI motility. If a species-appropriate, moist food fed in timed meals does not resolve the problem.
Identifying Food-related Problems
When there is nausea or vomiting, if kitty is diagnosed as having Inflammatory Bowel Disease and/or Pancreatitis, then food sensitivities/allergies need to be ruled out as a cause. Many traditional vets recommend “Novel proteins,” “Limited ingredient diets,” “Allergan-free diets” or “Hydrolyzed protein diets,” many of these being prescription diets. The problem? This approach is the equivalent of throwing spaghetti at the wall to see what sticks, and many of these foods have a poor ingredient list for long term use. It is much, much simpler to stop ALL commercial food and feed kitty a simple, meat-only bland diet short term. Think of it as plain chicken soup for a person with the flu.
The Bland Diet. If your cat is frequently nauseous or vomiting (or has diarrhea and parasites have been ruled out), consider stopping ALL food and treats, and feeding a bland diet (even better if with a novel protein) for a week or two (less in young kittens. Some vets approve this unbalanced diet for up to a month. Please discuss this with your vet). In cats, this is either a prepared meat-only baby food or a meat you poach at home. This bland diet is NOT nutritionally balanced and is for SHORT TERM USE ONLY. But just as drinking only chicken stock does not hurt us while we have the flu, eating just plain cooked meat will not harm your cat for a few days or few weeks. It is immensely helpful in quickly identifying if the food they’ve been eating is causing the problem.
In the U.S. the best baby food option is Beechnut or Goya as they are made with the water the meat and bone are cooked in (and then the bone is removed). This is the “broth” in the ingredient list. No, it is not seasoned with anything. Neither brand uses corn starch as a preservative (Gerber does). Consider using the turkey as your kitty has likely had less exposure to this protein vs chicken. The stage I, meat-only baby foods contain no spices or seasoning. If poaching a meat at home, it is important to include the water in which the meat was poached as part of the meals. The meat can be fed shredded in some of the broth, or the broth and meat can be blended together. Consider using boneless pork, as this is very likely a “novel” protein for your cat. Kitty won’t eat it? Try a different protein. If the nausea was severe, you may have to assist feed your cat for a day or two to give the bland diet a chance to settle the tummy. If problems continue or worsen, try a different meat before giving up. Cats are very strong creatures, but also idiosyncratic, as most kitty companions know very well.
Make and feed bone broth as a supplement to the bland diet. Bone broth is both nutritionally dense and yet extremely easy to digest. It is very healing and very soothing. In fact, you may need to feed bone broth for a day before kitty feels like eating the bland diet on her own. (Caution: Do not let your cat eat only bone broth for more than a day, and if your cat has liver disease, has been diagnosed with Inflammatory Bowel Disease or pancreatitis, do not let them go without food for more than 12 hours at most. Cats need close to their full complement of daily calories to prevent a liver disease caused by not eating, called hepatic lipidosis or “fatty liver.” The treatment for fatty liver is food. So best just to ensure kitty gets all they need in the first place). For bone broth instructions, see Dr. Becker’s video or transcript (if a chicken allergy is suspected, make the broth with bone-in turkey or pork or beef. There is no need to cook the larger bones to complete mush). Susan Thixton of Truth about Pet Food has written up a nice piece on the benefits of bone broth, though I do recommend following the instructions of the two-stage process that uses meaty bones as described by Dr. Becker, and keeping out some of the meat broth from Stage I before continuing to Stage 2. Some cats do not like the stage 2 broth. That’s fine, the meat broth is also very nourishing and soothing.
Has kitty improved on the bland diet? Then you know food is the problem. At this point, you MUST think of food almost as a medicine: food is the key to your cat’s health and happiness. Food can help heal or hinder the well-being of your cat. You can start trying different commercial canned foods, or you can just go straight to a commercial raw product for a minimally processed, fresh food option. Of course, making homemade fresh food where you control the ingredients is an option. It is more than just offering meat, but it isn’t rocket science.
Do not be surprised: Kitty may not like the food you make. Yes, this is disappointing, of course! But if all I’d ever eaten was dry cereal or canned stew, I probably wouldn’t like a salad or fresh fruit. It looks weird, has a strange texture, the temperature is likely different. So if kitty doesn’t take to the food right away, you need to give kitty time to transition. They will come to like, even love the food. They just need time. Transition help is available here.
As to making your own food, there are many ways to do this: cooked or raw; chunky meat and organs with bone-in meals (called “prey model raw”); an easy properly balanced vitamin premix added to meat or meat and liver. You may wind up wanting to move to prey model raw if feeding ground, or you may want to buy a grinder to manage making bone-in homemade ground. You may want to move to raw from cooked. There are no right answers here, these are all decisions of personal choice based on your lifestyle and your cat’s tastes and needs. None are particularly difficult; some approaches require investment in kitchen equipment. But when food is the problem, making one’s own and transitioning kitty with a slow introduction is often much easier in the long run than getting back on the food merry-go-round.
Do be aware, if you begin making homemade, it is important to include at least three proteins in rotation so that your cat does not develop a protein allergy/sensitivity and so that kitty does not reject the food due to boredom. Yes, even in your cats with IBD, these different proteins can be alternated at every meal, or every day, or every week. They do not need to be fed months at a time. Many kitties, once on raw, prefer the variety when offered more frequently.
Finally, it bears repeating: feeding a homemade diet is not just offering up meat. Cats need the minerals from bone and the dense nutrition in organs, and these need to be fed in proper proportion. Far too often we see people feeding just meat thinking they are doing something great for kitty, but this is a recipe for disaster. Here we’ve pulled together a list of approaches and recipes that are nutritionally balanced. All are simple and straightforward. They range from needing a grinder that can handle bones, to simply needing a food scale.
Please see the recipe for Easy Home Cooked Cat Food using a supplement premix that makes just meat and liver (in proper proportions) balanced and complete. The posted recipe is for making cooked food for kitty, as not everyone wants to feed raw. But please know the supplement used in this recipe was designed for balancing raw food, it just also balances cooked food. So the same recipe can be used to make raw or cooked food. If making raw, simply do not cook the meat and liver! Does not require a grinder, but does require a food processor and potentially a slow-cooker (though meat and liver can be cooked on the stove or in an oven, just use ALL of the water or pan drippings).
In Summary
As with people, in cats food is very frequently the root cause of nausea and vomiting (and for those with it, their diarrhea). Medicine is not the best answer when food is the problem. Medication is an important tool, and has its proper time and use. But altering what, how, and/or when we feed is often all that is needed to make kitty feel better. Feeding fresh food where we control the ingredients is sometimes needed, but in this author’s opinion, always preferable. Our cats are obligate carnivores. Their physiology is “designed” to have a low stomach pH and to eat primarily meat (bone and organ). Our cats are descended from desert animals and while some may drink water, cats do best when fed a moist diet, better yet, a fresh food diet. In many instances, identifying a problem ingredient can be difficult, and it is easiest to help our kitties feel better by simply getting off the commercial food merry-go-round. Transitioning is not always easy, but there are many tricks, tips, guides and resources to help. Persistence ALWAYS pays off. The road to good health is not a race, it is a journey.
Supplements, hydration, and medicines to manage ongoing problems with nausea that are not food related will be covered in Part 3.
And a shout out with thanks to Forrest D. Poston for the thoughtful input.
References
Funaba et al 2003. Effects of a high-protein diet versus dietary supplementation with ammonium chloride on struvite crystal formation in urine of clinically normal cats, Am J Vet Res, Aug; 64(8):1059-64 (2003). http://www.ncbi.nlm.nih.gov/pubmed/12926602
Funaba et al 2004. Evaluation of dietary carbohydrate on formation of struvite crystals in urine and macromineral balance in clinically normal cats, Am J Vet Res
Feb::65(2):138-42 (2004). http://www.ncbi.nlm.nih.gov/pubmed/14974568
Norsworthy et al 2013. Diagnosis of chronic small bowel disease in cats: 100 cases (2008-2012), J Am Vet Med Assoc, Nov 15;243(10):1455-61 (2013).
http://www.ncbi.nlm.nih.gov/pubmed/24171376
Plain English summary, by Gary Norsworthy, DVM for Veterinary Practice News, January 2014: Chronic Vomiting in Cats isn’t Normal After All.
http://www.veterinarypracticenews.com/Chronic-Vomiting-in-Cats-isnt-Normal-After-All/
Plantinga et al. 2011. Estimation of the dietary nutrient profile of free-roaming feral cats: possible implications for nutrition of domestic cats, British Journal of Nutrition / Volume 106 / Supplement S1 / October 2011, pp S35-S48.
http://journals.cambridge.org/action/displayAbstract?fromPage=online&aid=8404219
The Problem with Pepcid, Part 3: Healthy Supplements
and Alternatives for Treating Nausea
Laurie Goldstein, Oct 2015
This is the final part of a three part series. In Part 1, we discussed how long term use of antacids may raise stomach pH, which in turn can cause a number of health problems. In Part 2, we talked about how to identify nausea in your cat (including subtle symptoms), hairballs, and how food is a primary source of tummy (and other gastrointestinal) troubles in our cats.
As the primary cause of nausea and vomiting in our cats is food related, often managing nausea and/or vomiting in your cat is as simple as finding a non-kibble, meat-based, grain-free, low carbohydrate food that agrees with your kitty. Sometimes this doesn’t seem so simple as your vet or other cat parents offer suggestion after suggestion and your “picky” kitty turns up her nose at food after food. But the short-term use of a bland diet makes food-related identification simple and straightforward. This frequently resolves the problem if there isn’t an underlying disease. A bland diet doesn’t identify the problem ingredient(s), but if the food your cat has been eating is the source of the problem, a bland diet will identify that. At that point, controlling the ingredients with balanced homemade fresh food is easy, whether cooked or raw. Commercial fresh food (raw) products are becoming more widely available, and often a species-appropriate, less processed food resolves the problem. If it is a protein sensitivity, a single-protein fresh food diet in rotation will identify the allergy.
If the bland diet resolves the problem, great! We know how to proceed. If not, until – and if – we can identify the source of the nausea to treat it, or if kitty has a condition that requires ongoing nausea management, there are healthy alternatives to Pepcid a/c (famotidine) or Zantac (ranitidine) that may resolve the nausea without the potential long term use side-effects. These include:
For Immediate Relief
Slippery elm bark powder
Distilled or organic aloe vera juice (made from the inner leaf gel only)
Acupuncture
Proper hydration
B12
Longer Term Management
Probiotics
Digestive Enzymes
Any or all of these can be used together. In fact, probiotics, slippery elm bark powder, and the aloe vera juice (that contains no latex) work together synergistically.
Prescription Alternatives: Anti-emetic (central nausea) medications
Cerenia (maropitant)
Zofran (ondansetron)
We note that many cats are prescribed reglan (metoclopramide). This medicine increases muscle contractions in the upper digestive tract and triggers gastric emptying. This drug can be an important short term tool, but it causes serotonin syndrome and/or extreme anxiety and restlessness in many cats. Longer term use can cause an irreversible movement disorder.
Management of Nausea in Chronic Kidney Disease
For cats in chemotherapy or with chronic kidney disease (CKD), medical management may be necessary. Nausea in CKD is often ascribed to acid overproduction, but a study published in 2014 found this not to be the case. Cats, unlike dogs and humans, appear to suffer from central nausea, not gastritis related to acid overproduction. The study found “gastrointestinal signs noted in CKD cats may be more the result of uremic toxins and centrally acting emtogens than due to pathology within the stomach. The more common administration of antacids and gastroprotectants in cats may not be justified. … Management of gastrointestinal signs by use of antiemetic and antinausea drugs may be more worthwhile in cats with CKD.”
The two most commonly prescribed antiemetic drugs that treat central nausea in cats are Cerenia (maropitant) and Zofran (ondansetron). If one doesn’t work, try the other. Also, any of the alternative nausea treatments discussed here can safely be used in kitties with CKD. Fluids and B12 are likely already a part of their treatment plan.
Alternative Nausea Treatments
Slippery Elm Bark Powder
Slippery elm bark powder (SEB) is safe and non-toxic for cats. It may interfere with metabolism of medicine, so please give any meds at least 2 hours before or after giving it to your kitty.
Often SEB is all that’s needed to settle an upset stomach. As Dr. Hofve says, “It can be thought of as a sort of natural “Pepto-Bismol.” (Pepto-Bismol itself should not be used because it contains salicylate, a.k.a. aspirin). Its mucilage content coats, soothes, and lubricates the mucus membranes lining the digestive tract. Slippery Elm is an excellent treatment for ulcers, gastritis, colitis, and other inflammatory bowel problems. It is high in fiber, and so helps normalize intestinal action; it can be used to relieve both diarrhea and constipation. It may also help alleviate nausea and vomiting in pets suffering from non-GI illnesses, such as kidney disease.”
It is best if purchased as loose powder rather than in capsule form, as flow agents are required in the product when encapsulated. For nausea, it works best as a kind of “gruel” (gel) or “syrup” and given one-half hour to 45 minutes prior to a meal. Given kitty is nauseous and inappetent, you will most likely have to syringe it if made into a syrup, or spoon or finger feed it if used as a gel or “gruel.”
For the quick thick gel, mix one-quarter teaspoon of the powder with one-half teaspoon of water. Let it thicken. You may need to add water to get it into the syringe, that’s OK. Give 3 – 5ML (CC).
For the “syrup,” mix 1 teaspoon of SEB powder with one cup water. On the stove: bring to a boil, then let simmer for three to four minutes, whisking basically constantly. It will thicken as it cools. In the microwave: heat on high 30 seconds, stir. Repeat. Then cook it at 50% power for four minutes, stopping it every 20 to 30 seconds to stir so it doesn’t boil over. This can be refrigerated for up to 5 days, just take it out to use as needed.
For more information on slippery elm bark powder, please see:
Tips & Tricks
The Numerous Healing Properties of Slippery Elm
http://www.promedics.ca/site/downloads/Slippery%20Elm.pdf
Aloe Vera Juice (Distilled or from inner leaf only, no juice containing latex)
Aloe vera is well known for nutrient compounds that help heal and soothe the skin when used externally; it has similar benefits on the lining of the digestive tract when taken internally. Aloe decreases irritation and enhances healing and repair of ulcers in the stomach and intestines; it helps reduce intestinal inflammation. It can neutralize excess stomach acid without the pH rise associated with antacids over time, and it acts as a prebiotic, helping to promote the growth of healthy bacteria that aid digestion.
Up to twice a day, distilled aloe vera juice can be used in place of water to make the slippery elm bark gel or “gruel.” If not using SEB powder, one-half teaspoon of aloe vera juice can be given to kitty to drink or administered plain, via syringe, prior to a meal twice a day. It can also be mixed into food: this promotes healing longer term, but it doesn’t provide nausea relief if kitty isn’t eating.
Longer term, combining SEB powder, aloe vera juice, and a probiotic is an anti-inflammatory therapy that aids gastrointestinal health. To use this, mix one part SEB powder to 2 parts aloe juice (1/4 teaspoon SEB powder and 1/2 teaspoon aloe vera juice). Let it gel. Add and mix in the probiotic of choice. This can be given twice a day, and this can be added to food (if kitty is eating).
In the U.S. we suggest George’s or Lily of the Desert organic preservative-free unflavored juice. The organic is a bit bitter and kitty may not like it; the George’s has no taste but is not organic.
For more on Aloe Vera Juice, please see
Aloe vera and GI Tract Health
https://www.lorandlabs.com/pdf/Aloe%20Insight%20-%20Aloe%20vera%20and%20GI%20Tract%20Health.pdf
Health Risks & Benefits of Taking Aloe Vera Juice Internally
http://healthyeating.sfgate.com/health-risks-benefits-taking-aloe-vera-juice-internally-5017.html
Aloe Vera Gel Research Review
http://naturalmedicinejournal.com/journal/2012-09/aloe-vera-gel-research-review
Acupuncture for Nausea
To date, more than three dozen randomized controlled studies have been published showing that acupuncture point stimulation can treat or prevent nausea and vomiting. If you are in the U.S., you can search http://www.ahvma.org to see if there is a vet trained in acupuncture near you. I also recommend using an internet search to look for “holistic vets,” “Integrative vet,” “acupuncture vet,” etc. in combination with the name of your town, county, or nearby large city (if there is one). For the scientific-minded, this study (originally published in Hebrew) discusses how acupuncture works in managing nausea. How often your cat would benefit from the treatments will be discussed with the vet. But acupuncture in cats has proven to be very effective at helping treat nausea and usually results in an increased appetite.
Proper Hydration
Chronic vomiting or diarrhea, or a bout of vomiting or diarrhea can cause dehydration. Even subtle, mild dehydration can make your cat feel worse and exacerbate nausea. Sometimes fluid administration helps tremendously. This is obviously true for CKD cats who run the risk of dehydration due to improperly functioning kidneys and frequent urination. This may also help diabetic cats and cats with hyperthyroidism while you work to find the correct doses of medication to manage the diseases. Talk to your vet about administering sub-q fluids at home. If it is deemed safe and appropriate for your cat’s circumstances, having fluids on hand can make a real difference in how your kitty feels.
If you do not have sub-q fluids on hand, you can offer “tuna water” (drained from a tin of tuna); or slowly syringe plain water or coconut water (make sure it is unflavored with no preservatives). Coconut water is very similar in make-up to oral rehydration solutions, it contains properly balanced electrolytes naturally – but it does contain sugars. The use of children’s unflavored pedialyte is controversial due to the dextrose (sugar). Plenty of vets suggest it; others feel strongly the sugar is inappropriate for our obligate carnivores. But if your cat has been vomiting and is dehydrated and you don’t have sub-q fluids on hand, a homemade oral rehydration solution can get your kitty through the night and to the vet the next morning.
Oral rehydration solution: I make it by boiling, then cooling, one cup of water, and adding a small pinch of baking soda, a small pinch of salt, and a teaspoon of raw, organic honey. You can use a teaspoon of table sugar instead of the raw honey (do NOT use honey if it is not raw, the regular sugar is better). If the use of sugar, diluted, in such small amounts for a short period of time makes you uncomfortable, just syringe plain water and call the vet ASAP. But if you have a diabetic cat and your kitty is vomiting to the point of dehydration, if you can’t get to an emergency vet, that little bit of sugar may be a life-saver.
B12 Shots
For GI diseases that involve inflammation and malabsorption (such as inflammatory bowel disease, exocrine pancreatic insufficiency, pancreatitis, or intestinal lymphoma) or increased thirst and thus urination (such as hyperthyroidism, diabetes, or chronic kidney disease), B12 shots should be considered essential, in my opinion. Like fluids, vitamin B12 supplementation greatly enhances kitty’s well-being. B12 is water soluble, so even if B12 levels are not found to be low in blood work, your cat may benefit. It will not harm your cat to try, so ask your vet! https://ibdkitties.net/the-importance-of-b12/
Probiotics
Recent research has made it clear that we depend on our healthy bacteria for our health. In fact, our bacterial balance is so important to our immune system and digestive function, it can almost be thought of as another organ. A report published in September of this year put it this way “It is comparable to the immune system in as much as it is made up of a collection of cells, it contains a 100 times more genes than the host, is host-specific, contains heritable components, can be modified by diet, surgery or antibiotics, and in its absence nearly all aspects of host physiology are affected.”
Probiotics help us and our cats metabolize nutrients from our food, prevent the overgrowth of unhealthy bacteria, support almost every aspect of our immune system, regulate our moods, our weight, resolve and prevent allergies, regulate inflammation, and appear to help protect against several gastrointestinal-related cancers.
In the wild, a cat essentially gets a dose of probiotics with every meal. By eating the guts of its prey, kitty has a constant supply of bacteria to “feed” its gastrointestinal tract, its “microbiome.” The diet we feed our cats, even those feeding fresh food, is devoid of probiotics unless we supplement them.
Unfortunately, only limited data is available about the bacterial profile of cats. A May 2015 study of the fecal microbiome in cats with diarrhea was compared to healthy cats and significant differences were found: gut dysbiosis (the balance of GI bacteria) plays a very real role in the proper function of our cats’ GI system. Many recommend using “species-specific” strains of bacteria, as our cats do have bacteria that are unique to them. Ideally, we would provide bacteria derived from cats for best results. But so little is known about cat-specific species, one of the lead researchers in the field feels that probiotic selection for use in pets should be based on researched strains, not whether or not the probiotics are pet-specific, and indicates “studies have shown that human or dairy developed probiotic strains are capable of conferring health benefit across species. At this point there is no proven benefit of using a canine or feline specific strain.” Probiotics will not resolve nausea or vomiting in your kitty on a “per dose” basis. They are a supplement that usually works over time, not right away. Brands and doses for cats are discussed here: (insert link for ibdkitties)
Digestive Enzymes
According to Dr. Jean Hofve, “Digestive enzymes help our pets to fully break down foods so nutrients can be efficiently absorbed and used by the body. When food is not properly digested, some particles may trigger inflammation, allergies, and other chronic health problems. Processed foods have had their native enzymes destroyed, so it is important to add them to your pet’s food. Plant- or fungal-based enzymes work in the widest range of pH and temperature. Make sure that the product you select contains at least protease, amylase, lipase, and cellulase.” Fat malabsorption is a common problem for cats with brewing GI issues. This is often a cause of gas, discomfort, and stinky stool (usually in the form of diarrhea). Kitty should be taken to the vet for blood work to rule out Exocrine Pancreatic Insufficiency (EPI), and https://ibdkitties.net/pancreatitis/epi/. But in the absence of EPI, digestive enzymes can greatly benefit kitty’s GI health, comfort, and nutrient absorption.
For more information, please see
Digestive Enzymes http://ivcjournal.com/digestive-enzymes/
Summary
Digestive problems are so widespread in cats, according to VPI Insurance, they have ranked as one of the top two reasons for a vet visit seven out of the last nine years. Nausea and inappetence – “pickiness” in our cats – is not something to be taken lightly. One retrospective study of 100 cats with a history of chronic vomiting, weight loss, chronic diarrhea or a combination of those, found that 99 of those cats had either cancer or inflammatory bowel disease. Plenty of jokes abound about what we perceive as our haughty feline companions, or we write off our kitty’s problem as “just” hairballs or “he’s just a puker.” Cats should not be puking, they should not be sensitive to foods, and they should not be tossing hairballs with any frequency.
In some cases, the reputation of our “picky” eaters is merited: but for many, that pickiness we observe is actually a communication and the first indication that something isn’t right. Picky kitties are often actually at least slightly nauseous kitties. Clearly the first step is a visit to the vet. But if no underlying disease or cause is found, please remember as discussed in Part 2, the food we feed is often the culprit. If food changes as outlined don’t help, or if there is underlying disease that requires management of nausea, we hope these nausea management approaches help minimize the need for the use of antacids. Antacids are an important tool in the medicine chest, but it is best for kitty’s long term health to use them sparingly if possible.
References
Eamlamnam et al 2006. Effects of Aloe vera and sucralfate on gastric microcirculatory changes, cytokine levels and gastric ulcer healing in rats, World J Gastroenterol Apr 7; 2(13):2034-9 (2006).
http://www.ncbi.nlm.nih.gov/pubmed/16610053
Hofve, Jean DVM. Digestive Enzymes, IVC Journal; Spring 2012.
http://ivcjournal.com/digestive-enzymes/
Humphries C. 2015. The Deep Symbiosis between Bacteria and Their Human Hosts is Forcing Scientists to As Are We Organisms or Living Ecosystems? Seedmagazine.com October 11, 2015.
http://seedmagazine.com/content/article/the_body_politic/
Kumar et al 2010. Cancer-preventing attributes of probiotics: an update, Int J Food Sci Nutr Aug; 61(5):473-96 2010.
http://www.ncbi.nlm.nih.gov/pubmed/20187714
Marchesi et al 2015. The gut microbiota and host health: a new clinical frontier, Gut Sep:1-10 2015.
http://gut.bmj.com/content/early/2015/09/02/gutjnl-2015-309990.full
Marshall-Jones ZV 2006. Effects of Lactobacillus acidophilus DSM13241 as a probiotic in healthy adult cats, Am J Vet Res Jun;67(6):1005-12 (2006).
http://www.ncbi.nlm.nih.gov/pubmed/16740094
McLeland SM & Lunn KF et al 2013. Relationship among serum creatinine, serum gastrin, calcium-phosphorus product, and uremic gastropathy in cats with chronic kidney disease. J Vet Intern Med. May-Jun; 28(3)827-837 (2014).
http://www.ncbi.nlm.nih.gov/pubmed/24628683 and please see also
http://www.winnfelinefoundation.org/education/cat-health-news-blog/details/cat-health-news-from-the-winn-feline-foundation/2015/01/16/uremic-gastric-changes-in-cats-with-chronic-kidney-disease
Reynolds BC, Lefebvre HP. Feline CKD: Pathophysiology and risk factors—what do we know? J Feline Med Surg Sep; 15 Suppl 1:3-14 (2013).
http://www.winnfelinefoundation.org/education/cat-health-news-blog/details/cat-health-news-from-the-winn-feline-foundation/2015/01/16/uremic-gastric-changes-in-cats-with-chronic-kidney-disease
Samuels N. Acupuncture for nausea: how does it work? Harefuah Apr; 142(4):297-300, 316 (2003).
http://www.ncbi.nlm.nih.gov/pubmed/12754882
Sierra-Garcia GD et al. 2014. Acemannan, an extracted polysaccharide from Aloe vera: A literature review, Nat Prod Commun Aug; 9(8):1217-21 (2014).
http://www.ncbi.nlm.nih.gov/pubmed/25233608
Suchodolski JS. 2011. Companion Animals Symposium: Microbes and gastrointestinal health of dogs and cats, J Anim Sci 89:1520-1530 (2011).
https://www.animalsciencepublications.org/publications/jas/pdfs/89/5/1520?search-result=1
Suchodolski JS. 2015. Probiotics in GI Health, Western Veterinary Conference Proceedings S22C, 2013.
https://www.facebook.com/groups/RawFedIBD/1440619959508838/
Suchodolski et al 2015. The Fecal Microbiome in Cats with Diarrhea, PLoS ONE 10(5): e0127378 May 2015.
http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0127378
Wynn, SG 2009. Probiotics in veterinary practice, JAVMA 234(5):606-613 (2009).
http://www.winnfelinefoundation.org/education/cat-health-news-blog/details/cat-health-news-from-the-winn-feline-foundation/2009/04/02/probiotics-for-cats



 On the left:
On the left: